For Education
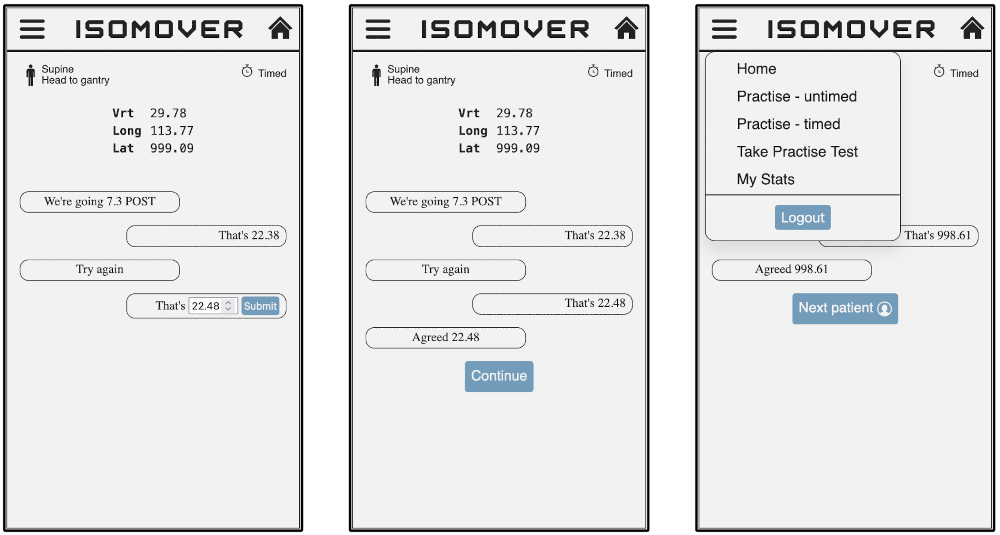
Isomover has been designed to allow realistic timed and untimed calculation practice, with minimal effort
required from educators to get their students up and running. University education teams and practice
educators can also administer tests to assess learning gain.
In 2018, Health Education England identified the need to grow the therapeutic radiography workforce by 45%
by 2027 to meet forecasted demand for radiotherapy and to improve cancer care.1
In response, intake onto therapeutic radiography courses has been increasing.2
However, the Society and College of Radiographers has warned that the availability of clinical placements limits
expansion.3 Furthermore, staff shortages, combined with increased demand
on service provision, impacts the ability of radiotherapy departments to meet the educational needs of students
while maintaining the quality of patient care.4
A possible release valve for such pressures is increasing the use of simulation in higher education institutions
(HEIs). Simulations of clinical practice are already used to bridge the gap between theory and practice for
therapeutic radiography students, most notably with the Virtual Environment for Radiotherapy Training
(VERT).5 6
It has been suggested that up to 20% of clinical placement can be replaced with such simulation.5
Further to this, specific areas of clinical practice for which simulation could be the most useful in developing
skills among pre-registration students have been highlighted in recent guidelines published by the Society of
Radiographers (SoR).7
A need for academics to be able to offer simulation as part of teaching delivery has
been identified in the College of Radiographers’ updated Education and Career Framework, solidifying its role
in the curriculum.8
The emphasis on simulation must be supported, however, by real-world evaluations of efficacy. Technologies
such as VERT have been evaluated in this way. For example, Ketterer conducted a randomised control trial
with first-year students, with 16 undertaking a two-week simulated placement and 13 attending a traditional
clinical placement.9 A subsequent formative assessment demonstrated a
parity of outcomes, though the simulation group scored over 10% higher on communication skills. As Ketterer
notes, the HEI involved faced a considerable financial outlay to create a meaningful simulated placement,
although repeating the programme could provide some economies of scale.9
 Practise without pressure
Practise without pressure
 Choose a difficulty level
Choose a difficulty level
 Take practise tests
Take practise tests
 Track your stats
Track your stats